Cataract Surgery: How Does The Brain Assimilate Visual Changes?

Although cataracts have been considered the leading cause of blindness worldwide, there is a simple surgical intervention that eliminates the problem and restores vision in affected people. However, this cataract operation contains a series of complexities that are interesting to know.
Eye cataracts are a fairly common visual problem. In fact, according to various studies, more than 60% of the world’s population from the age of 75 will develop some type of cataract. Therefore, cataracts are perceived as a threat as the years go by.
In addition, the symptoms of this ocular pathology are part of popular knowledge: people who suffer from them suffer a progressive impairment of the functionality of their vision that can become disabling.
What is a cataract?
What is clinically understood by ocular cataract is nothing more than the opacification of the lens. The lens is the transparent lens inherent in the eye by virtue of which it can focus, which is located behind the iris and the pupil.
When cataracts appear, this lens becomes progressively cloudy; due to an accumulation of epithelial cells that change color for pathological reasons.
These cells proliferate and prevent the normal passage of light through the lens, given that due to their translucent features and their brown hue, they represent a physical barrier for this passage. It’s like looking at the world through a foggy windshield. In this way, vision is affected.
There is another clinical picture: secondary cataracts. These are a pathological ocular state very similar to the previous one. It arises after the surgical removal of the cataract and is due to remnants of that darkened epithelium that have remained latent and have proliferated again, opacifying the structures of the eye again.
The resulting symptomatology is similar to that caused by primary cataract, but the eye injury is milder and less extensive. Thus, all that is required for its correction is the removal of that layer of tissue by laser. It is a quick, painless and risk-free procedure.
As a consequence of the formation of the cataract, in a progressive way -and more or less quickly depending on the type of cataract in question-, the affected person will experience the following visual discomforts:
- Decreased visual acuity.
- Photophobia and glare.
- Alteration of color perception – colors lose intensity and melt.
- Alteration of the perception of the surrounding space.
And, in general, any visual modification that may arise as a result of the light reflected by objects not being able to penetrate the eye or, if it does, it is obscured and distorted.
In addition, as an added confounding factor, while the cataract is in the process of extension, the different degrees of dilation or contraction of the pupil may mask or exacerbate the symptoms.
Thus, if the pupil is very dilated, much of the light that enters the eye will ‘avoid’ the cataract and the vision will be closer to normal. Now, if it is very contracted -in low light environments-, the light will meet the waterfall on its way and the vision will be very poor.
Causes of ocular cataract
Of all the causes, the most widely accepted is the body’s normal aging process. In this sense, developing cataracts would be a logical consequence of reaching advanced ages, although it is true that only susceptible people will develop them.
In a number of cases, the cause is genetic and the problem is called a congenital cataract. Therefore, there is a small percentage of babies born with this deficit. For our peace of mind, surgical correction is indicated at that age and the results are usually good.
In addition to the above, and leaving aside those conditions of unknown or unknown origin (idiopathic cataracts), three other causes are postulated as a possible origin of this oculopathy:
- A high degree of myopia -which influences ocular morphology-.
- Eye trauma.
- Prolonged steroid-based pharmacological treatments, especially corticosteroids -as occurs with chronic cortisone intake in rheumatism or antiallergic drugs in people with allergies-.
Whatever the cause of this problem, the result impacts in such a way on the daily performance of the person that suffering from cataracts usually brings with it a whole constellation of psychological ailments, among which anxiety and depression stand out.
What is the cataract operation?
Considered a simple and safe surgical intervention and given its ambulatory nature, this is a type of surgery that should not scare us. Hundreds of them are practiced a day around the world and the success rate is very high.
In summary, the intervention consists of the physical extraction of the cataract using instruments that are inserted in the anterior part of the eyeball.
Since the tissue to be removed is adjacent to healthy ocular tissue – and specifically, the lens – it is necessary to fully or partially remove the lens. In this way, the eye is aphakic or without the ability to focus on its own. Let us remember that it was the crystalline lens, our natural lens, which allowed this focus and, therefore, the accommodation of sight.
To make up for this structural and functional deficiency, an intraocular lens (IOL) is implanted in the space previously occupied by the lens, which allows the images to be focused, with characteristics that complement those of the IOL of the contralateral eye.
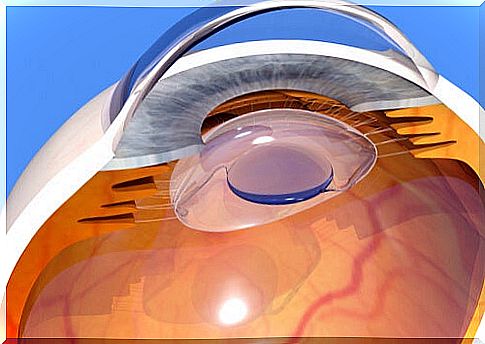
This is so because cataracts are almost always bilateral affections, that is, they occur in both eyes at the same time; to, together, form light projections focused at the level of the retina, which will then give rise to the visual representation, at the brain level.
But as is well known, on many occasions the artificial can hardly replace the natural. For this reason, IOLs, being artificial lenses that also remain fixed and do not have the ability of the lens to modify its shape to focus and defocus, profoundly alter and at various levels, the way the visual system works.
And the person in charge of constituting a final perceptual image, which is none other than the brain, must readjust to this new way of receiving light that will be transformed into images. For this reason, it may take up to a month for those intervened to complete this readjustment. Meanwhile, his vision is more imprecise and uncomfortable than before.
It is thanks to brain plasticity, to the ability of our neural systems to reorganize and adapt and recover lost functionalities, that this readjustment process culminates successfully and a good visual capacity is once again enjoyed.
Next, we list a series of components of the visual process that can be altered after cataract surgery. These are alterations that the brain will learn to correct in order to achieve a visual system that is as effective as possible.
Changes the brain must learn to integrate
Permanent focus and focus time override
Since IOLs only focus and cannot vary the degree of said focus, from the moment you have your eyes open you can see in a focused way at any distance, near or far; without having to strain your eyes, or let a few thousandths of a second pass until your gaze defocuses from one point and focuses on another.
This situation causes sensory strangeness at first, but over time this distortion normalizes.
Need for more light to see properly
Whereas when you suffer from cataracts, you tend to avoid highly luminous spaces, since they dilate the pupil and cause visual discomfort; After cataract surgery, that is, the implantation of IOLs, the brighter the environment, the better the focus and vision will be produced.
And this occurs mainly because the artificial lens does not cover the full diameter of the pupil when it is very dilated; so if it is, some of the light enters the eye from the outside of the IOL, causing double or blurred vision and halos.
Need for physical guidance
Since IOLs focus in a fixed and constant way, to adjust our vision to objects that are at a specific distance and with a position relative to us, we will not have the adaptation capacity of the lens but rather we will be the ones who, moving and By placing the head at different angles, let’s find the point of greatest visual acuity for that particular object.
Residual presbyopia
Generally, IOLs are more specialized in targeting medium and long distances and are less efficient for short ones. Therefore, it is not uncommon to need magnifying glasses after cataract surgery.
Visual changes to physical efforts
IOLs have a lower degree of fixation within the eye than the lenses did in their natural state.
For this reason, marked variations in the level of intraocular tension – the pressure exerted by liquid substances within the eye – that are produced as a consequence of physical efforts, will produce slight transient displacements of the lens that will cause distortions of the perceived image.
Tendency to eye irritation
The ocular or conjunctival epithelium, after having suffered ruptures by surgical intervention, develops microscopic scars that will increase the degree of sensitivity of the eye to irritating agents of the environment, such as smoke, dust, etc.
Different visual convergence
A complete final image is formed by merging two images of the same object, one from each eye.
Since IOLs are positioned somewhat differently than the original lenses, the exact point on the retina to which they project light is also different.
In this way, the two images to be fused to form a final image will come from different places, and the brain will relearn how to perform this fusion effectively.
Distortion of the visual plane and the sizes of objects
In general, IOLs implanted after cataract surgery produce a more flattened perception of the visual field, so that the initial objects appear less rounded.
Furthermore, they tend to dwarf the image they are focused on, so that objects in the world appear smaller than before. To all this, the brain must become accustomed to avoid generating visual discomfort as a consequence.
Presence of visual artifacts
By artifact in Medicine it is understood the presence of any element that should not naturally be found in a certain place. In the area of ophthalmology, a visual artifact would be an element that is presented in the context of the functioning of the visual system and that does not have to appear.
Specifically, IOL wearers can, under certain circumstances, perceive some components of the lens itself or even its movement.
This is uncomfortable and disconcerting and, sometimes, takes away attentional resources by being so striking. Again, getting used to the new visual situation, thanks to neuroplasticity, will make this less of a problem.
Whether you have had cataracts or if you are suffering from them or even if there is the possibility of developing them at some point, these are some important points that, in addition to being interesting in themselves, are useful to know to explain some of the results of cataract surgery , and above all for personal preparation prior to the intervention.